This is a guest blog submitted by Kat Suchet, the creator of Hatch Athletic.
If you’re expecting and want to keep up your weekly sweat seshes, you’ve probably already learned that you’re going to need to adapt slightly. The problem? There are too many myths about training pregnant that might have you confused.
There’s a lot of pregnancy fitness advice out there. Too much, in fact. A lot of it tends to tell you to “just keep moving as you’ve always done” and “listen to your body.” Plenty will tell you that it’s safe to do “moderate exercise.”
But what is moderate exercise anyway?
This advice isn’t tailored for the highly athletic population. In fact, the only scientifically researched advice is based on a population that has never lifted more than 20kg from the floor. That’s our warm-up weights!
The fact of the matter is there’s a distinct lack of solid research that goes beyond that.
I’m Kat, a physiotherapist, CrossFit coach, athlete, mum, and owner of Hatch Athletic. I’ve taken it on myself to dive into it over the last 2.5 years: to learn from women’s health physios around the world, unpick the available research, and look at the emerging work from pioneers out there.
It’s time to debunk the fact from the fiction about high-intensity functional exercise in pregnancy.

Myths About Training While You’re Pregnant: 5 We NEED to Debunk
Myth 1: You Should Keep Doing What You’ve Always Done
When I became pregnant, I had been a competitive CrossFit athlete and coach for going on five years. I was used to having control. I was used to manipulating my body, my diet, and my rest, and seeing results. I had been bossing it in the gym. In fact, I was probably the fittest I’d ever been, and now I couldn’t straddle the Assault bike for want of gagging or keeling over in a corner.
What was worse is all of the medical advice out there for the first trimester said I could work out as “normal.” The problem was, my normal was deadlifting double bodyweight and doing burpees to red-line… and I was seriously struggling.
My perfectionist tendencies meant I already felt inferior. Was I failing at being able to follow even the generic advice?
I think the best thing to say here is: You’re not the “normal.” CrossFit athletes, functional fitness athletes, and weightlifting women don’t really fall into a “normal” category of fitness, competitive or not. It’s easy to lose a bit of perspective when you’re doing it all the time, but even if you’re not a competitive athlete, if pre-pregnancy squatting under a 50, 60, 70kg barbell was your idea of normal, you’re actually very much an athlete.
Do not beat yourself up like I did. It’s okay if you can’t breathe and your barbell suddenly feels a lot heavier. Your body is doing an incredible thing and needs your energy elsewhere right now. Just getting to the gym is achievement enough — let it energise you, or let it help you zone out, or feel more normal.
Let me say this now. In the first trimester, it’s quite likely that you’ll be unable to perform physically in the way you are used to, despite the plethora of advice telling you that you can carry on with what you’ve been doing.
This is pregnancy safety advice, but what it neglects is the mental battle a fit female will go through when learning she simply can’t perform at the intensity that she is used to. Frankly, she’s knackered and can’t choose if she’d prefer to throw up or smash a bag of salty chips.
What you can or are allowed to do safely, and what you should give yourself permission to do, are two different things. Adjust your own expectations of yourself. Expect that you will achieve less in your first trimester.

Be humble in your approach to pregnancy exercise.
Myth 2: You’re a Goddess if You’re Still Smashing it in the Gym in Your 3rd Trimester
“Hmm? What? No ego here,” said no one ever.
I’m afraid if you’re sporty, then the two kind of come hand in hand to a greater or lesser extent. It means you’re competitive and you get a kick out of doing better each time than the time before — even if you’re competitive with yourself and not with others.
No More Exercises For Time
This is no longer a race. Don’t be tempted to ever choose intensity over the integrity of the movement. You’re now working out with different principles in mind.
My feeling is as most of us haven’t got a lot of experience exercising whilst pregnant, most of us can’t be absolutely certain we aren’t straining or overdoing it. So Mama, I’d say intensity should be the first thing to go. Your goals for exercise should now be about feeling good, maintaining your fitness levels and muscle mass, maintaining good posture and form, developing superhero pelvic floor control, and keeping gestational diabetes at bay.
If you are one of the lucky ones who feel energetic and is working out through your pregnancy comfortably, that’s great — but park the ego. It’s good to practice now: As pregnancy progresses, or as you head into delivery and the fourth trimester, you’ll have to make friends with slowing right down.
If you’re not managing to work out at all, that’s okay too. Don’t beat yourself up and fret over all the “lost fitness.” You are in such good shape for pregnancy, and that’s your job right now. The work you put in by being humble in your approach to pregnancy exercise will hold you in good stead for life.

This is no longer a race.
You should also steer clear of DOMs-inducing volume. DOMs (delayed onset muscle soreness) mean you’ve been lifting or exercising to the point of breaking and building new fibres. It’s largely present after a very high volume of reps or after some very heavy lifting. You aren’t building muscle mass anymore, and this should really be the last thing on your mind. No DOMS in later pregnancy is anything much to be proud of.
Which brings me nicely onto my next myth about training pregnant…
Myth 3: You Should Stay Below the 140bmp Heart Rate
This advice is now, thankfully, outdated. Yvonne Kelly, from Evoker Physiotherapy in Sydney, tells us all about exertion in pregnancy.
“We’ve got some pretty good research on the impacts of moderate, vigorous, and high exertion on fetal health, with the consensus on the need to avoid ‘high exertion’ as this can cause alterations in your growing bub’s heart rate (fetal bradycardia).”
High exertion means working at HR levels of >90% Max HR (Beetham, et al 2019). (Important to note this guideline is more like 60-80% Max HR for the sedentary woman, but I’m unlikely to find many of you here.) Therefore, the research indicates that exertion should be limited to <90%HR max for previously active women.
There has been no research on the effects above this point and should therefore be avoided. This serves as a clear HR ceiling to limit how hard you should push exercise through pregnancy.
Invest in a wearable device that has a decent heart rate monitor. Garmin, Whoop, MyZone, Polar, and now even FitBit and Apple Watch have all been clinically validated as accurate HR monitors.
Discomfort has become quite the norm in modern exercise. Oftentimes, pushing through discomfort is seen as an achievement. Use a monitor to remove the element of subjectivity.
But it’s not just HR… use the talk test too.
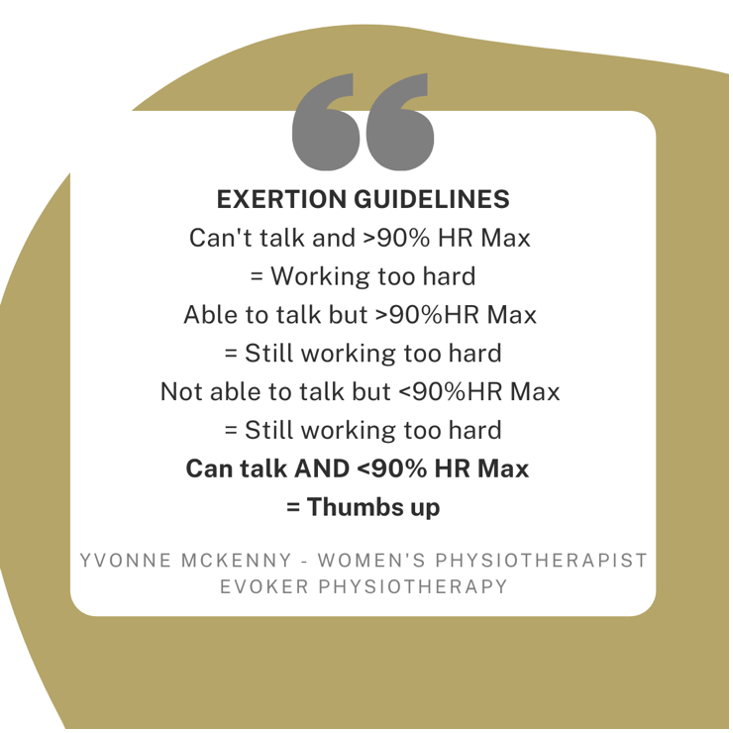
However, this is not without its own limitations. The somewhat inaccurate means of calculating HR max and the changes of HR in pregnancy — that is, an increase in resting and submaximal heart rate and ultimately the lack of research on the specifics — means that using HR alone can be insufficient.
For this reason, heart rate monitoring is recommended and best used in combination with the talk test. Simply put, if your breathing is strained such that you’re unable to hold a conversation or say more than a few words, you are likely working too hard and your baby is too.
This combined approach has been discussed in various papers (O’Neill 1991 and da Silva 2020) as the best way to navigate this somewhat grey area safely.”
Myth 3: You Should Be Afraid of Diastasis and Should Try to Avoid It
When I asked my community who was afraid of diastasis (DRA) in pregnancy, 93% came back with a yes. This makes me sad. It doesn’t need to be like that.
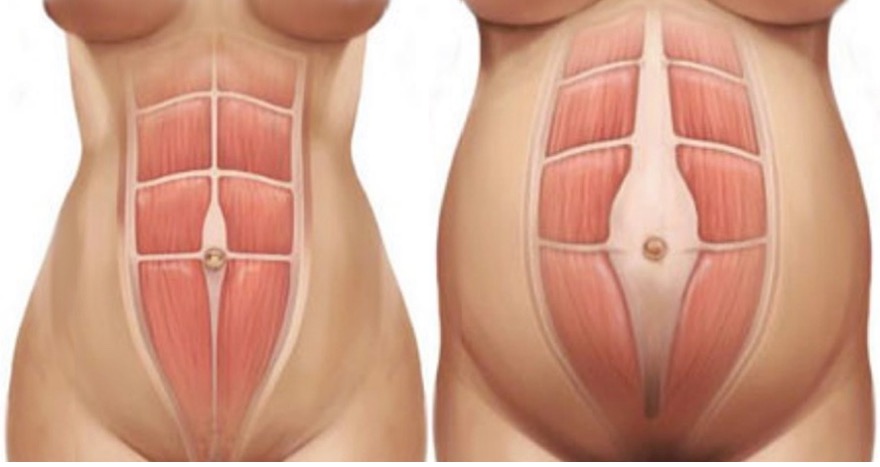
Diastasis is essentially when the abdominals separate to make way for your growing baby. They separate along a line of connective tissue called the linea alba. The abdominals don’t split — they move apart — and the linea alba widens and becomes stretched somewhat, but it doesn’t tear open.
The main take-home with diastasis is to watch for coning and do all you can to not put that connective tissue under any extra undue stress.
Coning is your body’s way of telling you that the linea alba — the connective tissue that connects your abdominals — is under undue pressure. Your belly will look cone-shaped, or there may be a little bulge from the middle section of your tummy or going up towards your ribs. Don’t panic if you see it. Just take that as your body’s way of telling you to stop that exercise for now.
Common movements which add undue pressure to the midline in pregnancy are:
- Prone loaded positions (planks, push-up positions, burpees, mountain climbers). Scale them to incline versions or stop them altogether, if need be.
- Abdominal loading exercises (sit-ups, v-ups, hollow holds, candlesticks).
- Hanging and pulling (overhead hanging exercises such as pull-ups, toes-to-bar, rope climbs, ski erg, and also sometimes horizontal pulling positions, like rowing).
Everyone is different. Keep watching your belly and be mindful to stop or change up certain movements if need be.
Going to see a women’s health physio will help you to learn what cues work for you to coordinate control and reduce coning in pregnancy (which will also stand you in really good stead for your postpartum journey too).
Another diastasis myth: “You can close your diastasis at any time postpartum.”

Many women will have a remaining DRA after they’ve given birth, and anything up to a 2cm gap is considered quite normal. DRA is often not down to anything you did or didn’t do during pregnancy. The latest opinion is that it’s mostly genetic and/or environmental (multiple babies).
Functional control of your diastasis means the ability to maintain tension across the gap. To do this, the correct coordination is key. By learning to coordinate the pelvic floor muscles, the core system, and the breath, we can protect ourselves from longer-term complications such as pain, continence issues, and pelvic organ prolapse.
The best time to try to rehab a diastasis is in weeks 0-6 postpartum. Yep, not many people tell you that, either. That’s because this is the time when we’re not meant to be doing any exercise, and this still stands. But there is one key exercise you can be doing, which is perfectly safe to do in those early weeks and which will help capitalise on the lasting springiness in the linea alba in early postpartum.
Post-partum programmes that claim they can close the gap are more than likely capitalising on a need to get that pre-baby body back. But the fact is if you’ve been careful in your training in pregnancy and there’s still a little gap at eight weeks post-partum, you’re more than likely looking at a longer-term diastasis. It’s just not that simple to close it.
But what you can do is make your core and midsection bulletproof. Having a fully functioning DRA with excellent tension shouldn’t stop you from doing anything whatsoever.
We have a more in-depth ebook on diastasis that you can download for free on our website here.
Myth 4: You Should Stop Lifting in Pregnancy

First things first: Don’t stop strength training! Keep going. In fact, strength training is probably the most important element to keep in your pregnancy programming. Now, we’re not talking one-rep maxes here. But from a physical standpoint, maintaining a level of compound strength can help with managing the increased demands on your skeletal system as you progress through pregnancy.
Being fit and strong as you head towards giving birth will undoubtedly stand you in excellent stead for managing your delivery and recovery too.
Squatting in particular helps with strengthening and conditioning the pelvic floor and reducing symptoms of pelvic girdle and back pain in pregnancy. However, as you go through pregnancy, you might find you need to alter the lift. Back squats can shift to front squats as your belly grows to reduce the strain on your spine, and the depth can reduce to a box squat.
Nicola Rutty, Physiotherapist from Stack Street Physiotherapy, says, “I’m afraid to say that pregnancy is not the time to be trying for a 1RM, or even a 2RM, for that matter. Avoid lifting heavy, heavy things. Keep things in a lighter zone where you don’t have to heavily breath hold or brace, which increases intra-abdominal pressure.”
“You should also be aware of the effect of the valsalva manoeuvre, or what we also call breath holding pre-lift, which can cause a rapid increase in blood pressure and decrease blood flow to the foetus.” Although unfortunately, the repercussion here on the foetus remains unknown (give us more studies please!) as a result, it’s better to avoid it excessively. Instead, learn to breathe for your pelvic floor on all resistance work.
Remember to prioritise form and posture over everything. When you’re pregnant, your centre-of-gravity changes considerably. Get friendly with your video and photo function on your phone and keep tabs on how you’re moving. If it starts to look dodgy, it probably is. Scale it back or choose a different movement.
Myth 5: If it Feels Okay, You Can Keep Going
A lot of the damage we can do to our bodies in pregnancy doesn’t even hurt. I err on the side of caution when it comes to high-impact exercises during pregnancy beyond the early second trimester. The reasons are multiple (and one size doesn’t necessarily fit all) but risks versus benefits must be weighed up when factoring in:
- Hormones (including those that relax your PF ligaments).
- Overheating and elevated heart rate.
- The pressure of bub on your pelvic floor.
Yvonne Kelly tells us, “The pelvic floor is now not only relaxing, but it has the increased strain and pressure from the mother’s increasing body weight and that of the growing baby. This is likened to 100kg of weight on your pelvic floor! And that’s without the added impact of running.”
And it’s not as simple as doing extra Kegels to counteract this. A large part of your pelvic floor isn’t muscular — it’s ligaments and fascia. Fascia damage is irreversible postpartum, so we need to do everything we can to protect it during pregnancy. My advice is as you start to grow bigger, swap box jumps for step-ups, running and double-unders for the air bike, and be wary of explosive movements in some lifts, i.e., jerks and snatches.
There’s so much more to it than this, and we have a whole article just on this topic alone. No matter what you decide, however, you should stop running/impact exercises if you experience any leaking, a feeling of heaviness or dragging in the pelvis, chest pain, headaches, dizziness, or severe shortness of breath.
Myth 6: In Your 3rd Trimester, it’s Mostly Air Bike

Nope, not true. It’s definitely not all doom and gloom! Our Hatch athletes have been very kind and shared below their favourite exercises as they hit the final stretches of their pregnancies:
Michelle: Squats
Natasha: Sumo deadlifts
Anthea: Light wall balls (can modify the depth of squat if need be)
Megan: Sled push
Kate: Assault bike
Gemma: Slam Balls
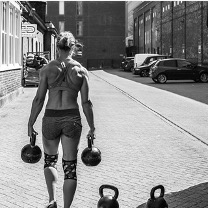
Kat: Farmers carries
Kelsey: Russian KB swings
Dee: Incline bench press
Laura: Tripod bent-over dumbbell row
Liv: Dumbbell hang power cleans
View this post on Instagram
For the most part, these will help you get those endorphins going in a safe, pelvis-friendly way. Please bear in mind this advice should never be substituted for medical advice and every pregnancy will be different. You may or may not have pre-existing conditions, injuries, or pregnancy complications. Of course, every athlete is different, and you’ll need to choose movements that are comfortable and safe for your individual circumstances.
Kat Suchet is the creator of Hatch Athletic, an online pregnancy resource for athletes and a postpartum training program specifically designed to get athletic mums back to the barbell. Hatch is designed not only for the athletic and competitive female, but it’s also the first holistic resource of its kind, helping new athletic mothers navigate pregnancy and postpartum not only physically but mentally too.
Kat is a physiotherapist, CrossFit athlete, and coach. She lives in Sydney with her partner Tom and 20-month-old Ralph. You can reach her at Kat@hatchathletic.com.
IG: @Hatch_Athletic
Facebook: @HatchAthletic